Introduction
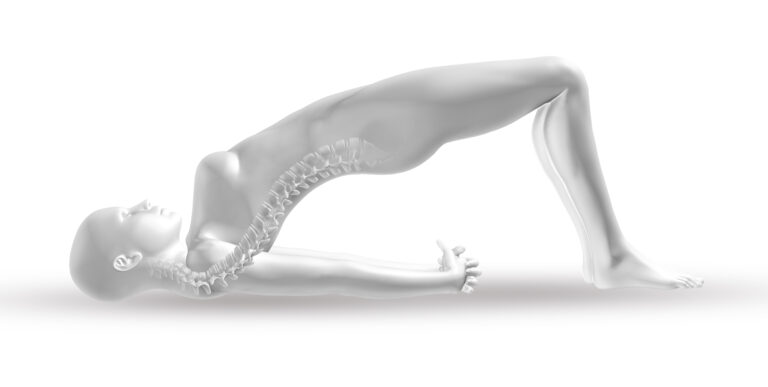
Menopause marks a significant shift in a woman’s hormonal balance, leading to a decrease in estrogen levels. This hormonal change can have a profound impact on bone health, as estrogen plays a crucial role in maintaining bone density. Post-menopausal women are at an increased risk of osteoporosis and bone fractures due to accelerated bone loss. Understanding the connection between menopause and bone density is essential for taking proactive steps to protect skeletal health during this phase of life.
Overview
During menopause, the decline in estrogen accelerates the breakdown of bone tissue, leading to a decrease in bone mass. As bone density decreases, bones become more fragile and prone to fractures. Women may experience thinning bones in the spine, hips, and wrists. To safeguard bone health, it is essential to incorporate preventive measures such as proper nutrition, exercise, and medical interventions to slow bone loss and enhance bone strength.
Potential Risks and Complications
- Increased Risk of Osteoporosis: Menopause-induced bone loss can lead to osteoporosis, where bones become porous and more susceptible to fractures.
- Fracture Risk: Fragile bones increase the likelihood of fractures, especially in the spine, hips, and wrists.
- Chronic Pain and Disability: Severe bone loss and fractures can lead to chronic pain, reduced mobility, and long-term disability.
Understanding the Recovery Process
- Medical Management: Hormone replacement therapy (HRT), calcium, and vitamin D supplements may be prescribed to slow bone loss and support bone health.
- Exercise and Rehabilitation: Weight-bearing exercises such as walking, dancing, or strength training help maintain bone density and improve balance, reducing the risk of falls.
- Monitoring Bone Health: Regular bone density scans (DEXA scans) help monitor bone health and assess the need for treatment adjustments.
Factors Influencing Outcomes
- Age at Menopause: Early menopause may increase the duration of bone loss, leading to a higher risk of osteoporosis.
- Lifestyle Choices: A diet rich in calcium, vitamin D, and regular physical activity can slow down bone loss.
- Medical Intervention: Early detection and appropriate treatments, such as bisphosphonates or selective estrogen receptor modulators (SERMs), can help manage bone health during menopause.
- Genetic Factors: A family history of osteoporosis or fractures may predispose women to bone density loss and fractures.
Informed Decision-Making
- Understanding Treatment Options: Women should be aware of available treatments, including hormone therapy, medications, and lifestyle changes, to make informed decisions about their bone health.
- Regular Health Monitoring: Routine bone density testing and regular consultations with healthcare providers are crucial for managing bone health during and after menopause.
- Adopting Preventive Measures: Women should prioritize calcium-rich diets, weight-bearing exercises, and other preventive strategies to protect their bones and minimize risks.
Key Takeaway
Menopause significantly impacts bone density due to hormonal changes, leading to an increased risk of osteoporosis and fractures. Women can safeguard their skeletal health by adopting preventive measures such as proper nutrition, regular exercise, and seeking medical advice for early intervention and treatment options.
Disclaimer
This information is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a healthcare provider for personalized guidance regarding menopause and bone health management