Baker’s cyst, also called popliteal cyst, is a common issue in the knee. These fluid-filled cysts form at the back of the knee, creating a lump that can cause stiffness and discomfort. The condition is named after Dr. William Morrant Baker, a surgeon from the 19th century who first talked about it. The cysts often happen because there’s a problem inside the knee joint, like arthritis or a tear in the meniscus. These conditions cause the joint to generate extra fluid, potentially resulting in cyst formation. Most baker’s cysts can get better without surgery.
Anatomy of Baker’s Cyst
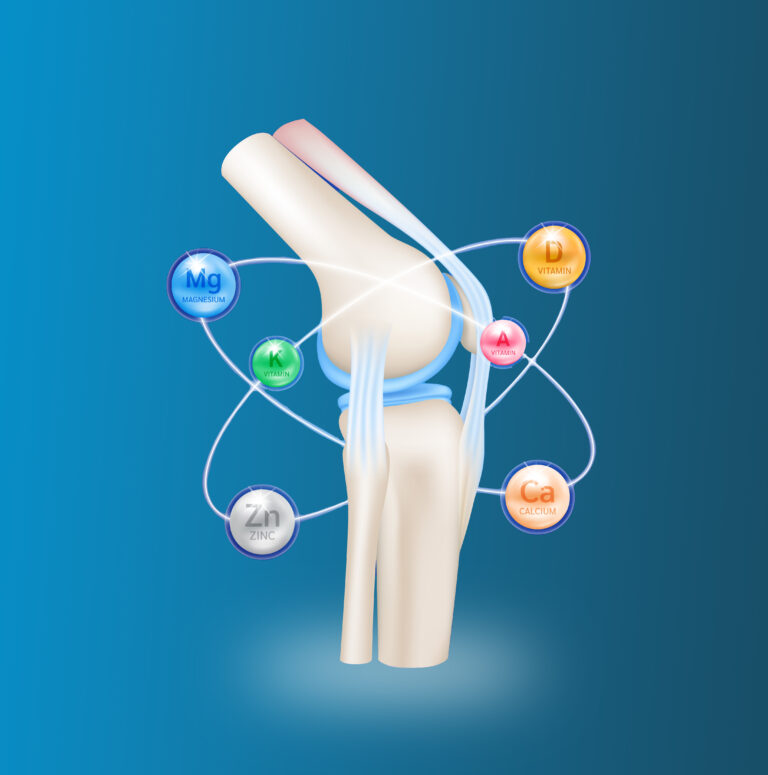
The knee is the largest and most robust joint in the human body. It’s made up of the lower part of the femur (thighbone), the upper part of the tibia (shinbone), and the patella (kneecap). It assists your doctor in obtaining a clearer view of the lump behind your knee and determining whether it consists of solid material or fluid. Inside the knee joint, there’s a clear fluid called synovial fluid, which serves as a lubricant to minimize friction within the joint. Small sacs filled with fluid, called bursa, cushion the joint and help decrease friction between muscles and other nearby parts.
Causes
In grown-ups, Baker’s cysts usually happen because of an injury or a condition that causes swelling and inflammation inside the knee joint, such as:
- Osteoarthritis
- Rheumatoid arthritis
- Meniscus tear
- Anterior cruciate ligament (ACL) tear
- Other problems that harm the tissues inside the joint
When the knee gets inflamed, it produces more synovial fluid, which goes behind the knee and builds up in the popliteal bursa. The bursa then swells and forms a Baker’s cyst.
Symptoms
Some Baker’s cysts don’t cause any symptoms and are only found during a physical check-up or when having an MRI scan for some other reason. When signs do occur, they may involve:
- Feeling a lump or fullness behind the knee
- Knee pain
- The sensation of rigidity or tension behind the knee
- Swelling in the knee and lower leg
If the cyst gets very big, it can affect blood flow in the leg’s veins. This can cause pain, swelling, weakness, or numbness if nerves are compressed. Very rarely, the cyst can burst. Sometimes, the symptoms of a cyst might seem like those of a blood clot or deep vein thrombosis, which is a much more serious issue. If you notice increasing pain and swelling in your calf, it’s important to get medical help immediately to rule out a blood clot.
Treatment Approaches to Baker’s Cyst
NONSURGICAL TREATMENT:
Most Baker’s cysts go away on their own. When cysts persist, initial treatment consistently takes a nonsurgical approach, potentially involving one or more of the following methods:
- Observation – Your doctor might suggest keeping an eye on the cyst to make sure it doesn’t get bigger and cause pain.
- Activity modification – Avoiding activities that put too much strain on your knee, like jogging and aerobics, can help ease symptoms.
- Anti-inflammatory drugs – Drugs such as ibuprofen and naproxen have the ability to alleviate pain and reduce swelling.
- Steroid injection – Your doctor might inject a corticosteroid into your knee to reduce inflammation.
- Fine Needle Aspiration – In this process, your doctor numbs the area around the cyst, then uses a needle to remove extra fluid from the joint. They may use ultrasound to help guide the needle accurately.
SURGICAL TREATMENT:
Surgery for a Baker’s cyst is rarely needed. But your doctor might suggest it if you have painful symptoms that don’t go away with nonsurgical treatment or if your cyst keeps coming back even after aspiration.
- Arthroscopy – Your doctor makes small cuts under anesthesia and puts a tiny camera called an arthroscope into your knee joint. The camera shows images on a screen, and your doctor uses them to guide small surgical tools.
- Excision – For big cysts or those causing nerve and blood vessel issues, your doctor might do open surgery to remove the whole cyst.
Conclusion: Understanding Baker’s cysts sheds light on the intricate dynamics of knee joint health. Recognizing that these cysts often stem from underlying joint conditions underscores the importance of proactive management and timely intervention. By embracing non-surgical approaches and, when necessary, judicious surgical options, individuals can navigate towards effective relief and recovery. Emphasizing the significance of early detection and comprehensive care, this journey underscores the invaluable role of informed decision-making and tailored treatment strategies in optimizing musculoskeletal wellness.
Disclaimer: The information provided in this blog post is for general informational purposes only and should not be considered professional advice. Before making any health-related decisions, consult with a qualified healthcare professional. The content is not a substitute for medical advice, and individual results may vary. The author and website are not responsible for any consequences arising from the use of the information provided. Use your best judgment and seek professional advice when needed.