Introduction
Osteoporosis is a silent disease that gradually weakens bones, making them fragile and more susceptible to fractures. Women, particularly postmenopausal women, are at a higher risk due to the hormonal changes that occur during menopause, which significantly affect bone density. The lack of noticeable symptoms until a fracture occurs often makes osteoporosis a hidden concern. However, understanding the causes, prevention strategies, and treatment options can empower women to take proactive steps in managing and preventing bone loss, leading to better bone health throughout life.
Overview
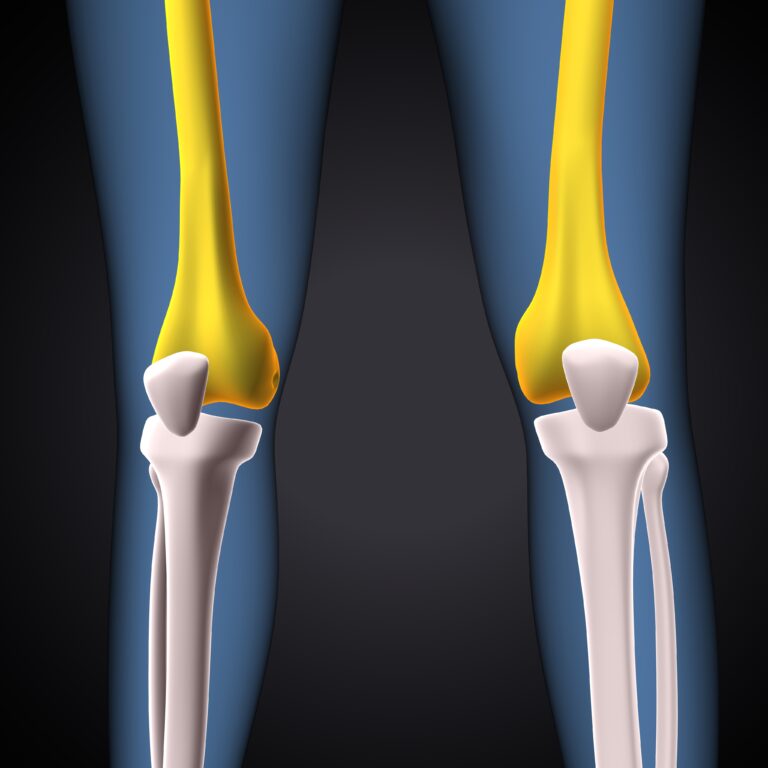
Osteoporosis occurs when the body loses too much bone mass, or makes too little bone, leading to porous, fragile bones. The decline in estrogen levels during menopause accelerates bone loss, making women more susceptible to fractures, especially in the spine, hips, and wrists. Preventing osteoporosis involves lifestyle changes such as diet, exercise, and possibly medications. Early intervention is key, as bone density loss can be slowed or even reversed with the right approach.
Potential Risks and Complications
- Increased Fracture Risk: Fragile bones are more prone to breaks, even from minor falls or injuries, leading to long-term disability and pain.
- Chronic Pain: Fractures or spinal deformities resulting from osteoporosis can cause persistent pain and discomfort.
- Decreased Mobility: The fear of falling and fractures can lead to decreased activity, worsening bone health and overall physical well-being.
Understanding the Recovery Process
- Bone Density Testing: Regular bone density scans (DEXA scans) help monitor bone health and track the progression of osteoporosis.
- Medication Management: Treatments like bisphosphonates, hormone replacement therapy (HRT), or selective estrogen receptor modulators (SERMs) may be prescribed to slow bone loss and increase bone density.
- Physical Therapy: Strengthening exercises and balance training are essential to prevent falls and improve bone strength.
- Lifestyle Adjustments: Proper nutrition with adequate calcium and vitamin D, along with regular weight-bearing exercises, can help manage bone density and prevent further bone loss.
Factors Influencing Outcomes
- Age and Menopause Status: Women who experience early menopause or are older are at a higher risk of developing osteoporosis.
- Lifestyle Factors: Diet, physical activity, and smoking or alcohol use can significantly influence bone health.
- Genetics: A family history of osteoporosis may increase the likelihood of developing the condition.
- Medical Conditions: Underlying health conditions such as rheumatoid arthritis or thyroid disorders can affect bone health and contribute to osteoporosis.
Informed Decision-Making
- Understanding Risk Factors: Women should be aware of their personal and family medical history to identify risks and take proactive steps.
- Exploring Treatment Options: Women should discuss medication options with healthcare providers to understand the risks and benefits of treatments available for osteoporosis.
- Adopting Preventive Strategies: Women should focus on diet and exercise, ensuring they receive sufficient calcium and vitamin D, and engage in regular weight-bearing activities to build and maintain strong bones.
Key Takeaway
Osteoporosis is a significant concern for women, especially after menopause, but it can be managed and even prevented with proactive steps. Regular screenings, a healthy lifestyle, and appropriate treatments can help women maintain bone density and reduce the risk of fractures. Early intervention is essential to safeguard bone health and prevent complications later in life.
Disclaimer
This information is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always consult with a healthcare provider for personalized guidance regarding osteoporosis prevention and management.